A closely watched Alzheimer’s drug from Eli Lilly won the backing of federal health advisers on Monday, setting the stage for the treatment’s expected approval for people with mild dementia caused by the brain-robbing disease.
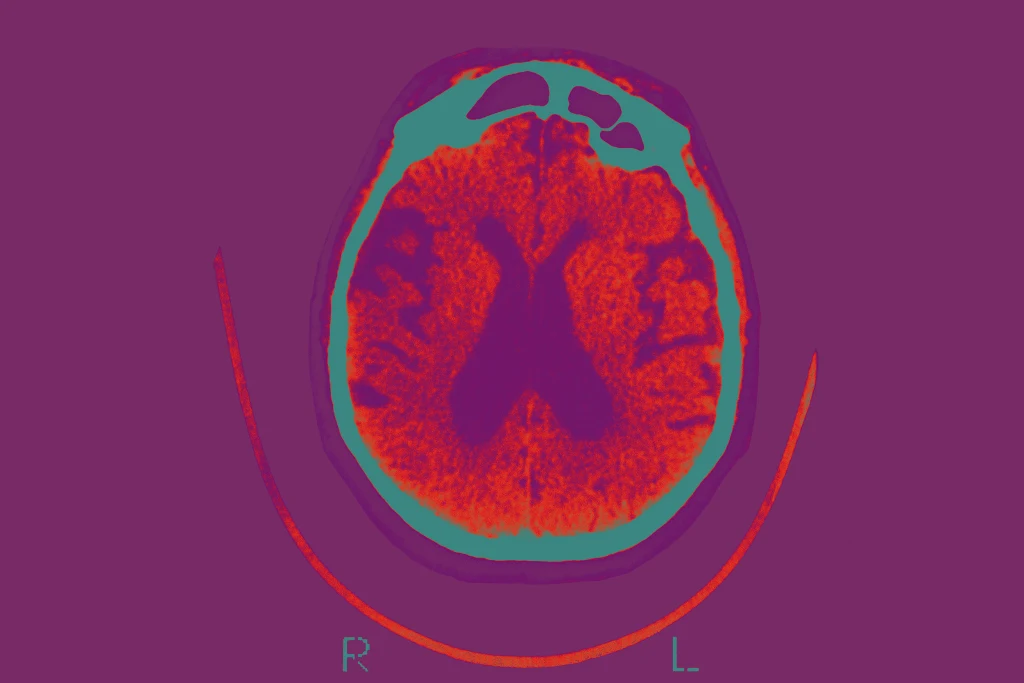
A panel of Food and Drug Administration advisers voted unanimously that the drug’s ability to modestly slow the disease outweighs its risks, including side effects like brain swelling and bleeding that will have to be monitored.
“I thought the evidence was very strong in the trial showing the effectiveness of the drug,” said panel member Dean Follmann, a statistician from the National Institutes of Health.
The FDA will make the final decision on approval later this year. If the agency agrees with the panel’s recommendation, the drug, donanemab, would only be the second Alzheimer’s drug cleared in the U.S. to convincingly slow cognitive decline and memory problems due to Alzheimer’s. The FDA approved a similar infused drug, Leqembi, from Japanese drugmaker Eisai last year.
In a separate vote, the FDA advisers voted unanimously that the Lilly drug was shown effective in various subgroups of patients.
Lilly studied its drug by grouping patients based on their levels of a brain protein, called tau, that predicts severity of cognitive problems. That prompted FDA reviewers to question whether patients should be screened via brain scans for tau before getting the drug. But most panelists thought there was enough evidence of the drug’s benefit to prescribe it broadly, without screening for the protein.
“Imposing a requirement for tau imaging is not necessary and would raise serious practical and access concerns to the treatment,” said Dr. Thomas Montine of Stanford University, who chaired the panel and summarized its opinion.
The FDA had been widely expected to approve the drug in March. But instead the agency said it would ask its panel of outside neurology experts to publicly review the company’s data, an unexpected delay that surprised analysts and investors.
At a high level, Lilly’s results mirrored those of Leqembi, with both medications showing a modest slowing of cognitive problems in patients with early-stage Alzheimer’s. The Indianapolis-based company conducted a 1,700-patient study showing patients who received monthly IV infusions of its drug declined about 35% more slowly than those who got a sham treatment.
But there were differences in the way Lilly tested its drug that raised questions for the FDA.
Patients with different tau levels showed varying degrees of benefit in Lilly’s study. But the company excluded patients with little or no tau, assuming their disease would progress too slowly to show a benefit.
That exclusion prompted FDA reviewers to question whether the drug’s benefits could be generalized to all patients — as suggested by Lilly — or if the drug should be limited to patients like those studied by the company.
Panelists said there was enough data from other measures to feel confident that all patients could benefit from the drug, regardless of tau.
There was another key difference in Lilly’s research that panelists considered.
Like other drugs in the class, Lilly’s works by clearing a sticky brain plaque called amyloid that’s a contributor to Alzheimer’s. But unlike Leqembi and other drugs studied, Lilly stopped administering the drug to patients once their plaque reached very low levels.
Lilly scientists have suggested stopping treatment is a key advantage for its drug, which could reduce side effects and costs of long-term use. But FDA staff said Lilly provided little data supporting the optimal time to to stop treatment or how quickly patients might need to restart it.
Despite those questions, many panelists thought the possibility of stopping doses held promise.
“It’s a huge cost savings for the society, we’re talking about expensive treatment, expensive surveillance,” said Dr. Tanya Simuni of Northwestern University. She and others experts said patients would need to be tracked and tested to see how they fare and if they need to resume treatment.
The main safety issue with donanemab was brain swelling and bleeding, a problem common to all amyloid-targeting drugs. The rates reported in Lilly’s study were slightly higher than those reported with competitor Leqembi. However, the two drugs were tested in slightly different groups of patients, making it difficult to compare their safety, according to experts.
Three deaths in the donanemab study were linked to the drug, according to the FDA, all involving brain swelling or bleeding. One of the deaths was caused by a stroke, a life-threatening complication that occurs more frequently among Alzheimer’s patients.
FDA’s panel agreed that those the risks could be addressed by warning labels and education for doctors as well as medical scans to identify patients at greater risk of stroke.